What Is Creatinine and Creatinine Clearance?
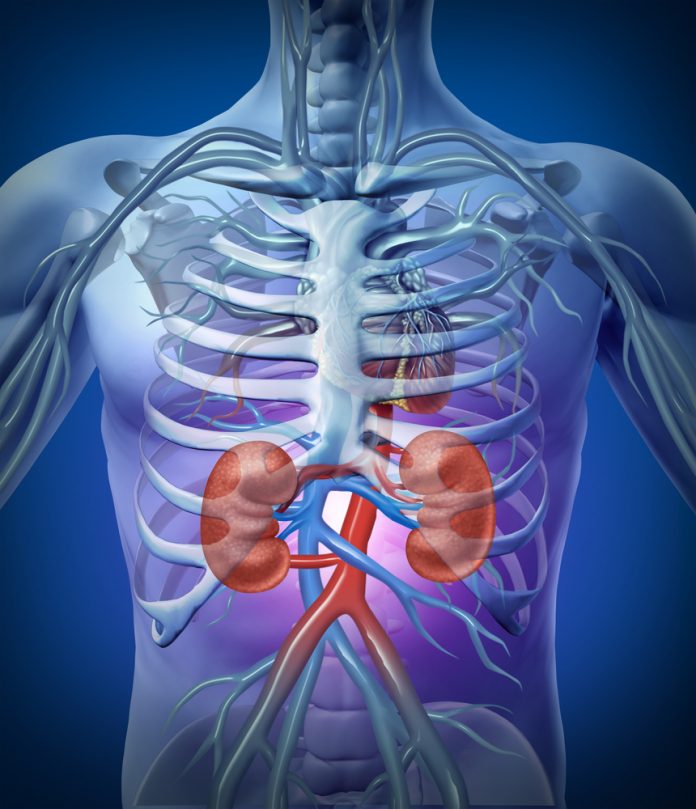
Creatinine is a waste product that is produced continuously during normal muscle breakdown. The kidneys filter creatinine from the blood into the urine, and reabsorb almost none of it.
The amount of blood the kidneys can make creatinine-free each minute is called the creatinine clearance. Creatinine clearance in a healthy young person is about 125 milliliters per minute — meaning each minute, that person’s kidneys clear 125 mL of blood free of creatinine. The GFR can vary depending on age, sex, and size. Generally, the creatinine clearance is a good estimation of the glomerular filtration rate.
Measuring Creatinine Clearance and Renal Function
Doctors use creatinine and creatinine clearance tests to check renal function (kidney function). Testing the rate of creatinine clearance shows the kidneys’ ability to filter the blood. As renal function declines, creatinine clearance also goes down.
There are two main ways doctors use creatinine tests to measure kidney function:
Creatinine clearance can be precisely determined by measuring the amount of creatinine present in a sample of urine collected over 24 hours. This method requires a person to urinate exclusively in a plastic jug for one day, then bring it in for testing. Although the urine creatinine measurement method is inconvenient, it may be necessary to diagnose some kidney conditions.
GFR can be estimated using a single blood level of creatinine, which your doctor enters into a formula. Different formulas are available, which take into account age, sex, and sometimes weightand ethnicity. The higher the blood creatinine level, the lower the estimated GFR and creatinine clearance.
For practical reasons, the blood test estimation method for GFR is used far more often than the 24-hour urine collection test for creatinine clearance.
A low GFR or creatinine clearance demonstrates kidney disease. The decline in kidney function can be either acute (sudden, often reversible) or chronic (long-term and irreversible). Repeated GFR or creatinine clearance measurements over time can identify kidney disease as acute or chronic.
Kidney function and creatinine clearance naturally decline with age. Fortunately, the kidneys have a huge reserve capacity. Most people can lose well over half their renal function without symptoms or significant problems.
Doctors determine the severity of chronic kidney disease with a staging system that uses GFR:
Stage 1: GFR 90 or greater (normal kidney function)
Stage 2: GFR 60-90 (mild decline in kidney function)
Stage 3: GFR 30-59 (moderate decline in kidney function)
Stage 4: GFR 15-29 (severe decline in kidney function)
Stage 5: GFR less than 15 (kidney failure, usually requiring dialysis)
People over age 60 may have an apparently normal creatinine blood level, but still have a low GFR and creatinine clearance. The 24-hour urine collection method, or one of the GFR estimation formulas, can more accurately identify the decline in kidney function.
How Do I Know If I Have Kidney Disease?
Blood and urine tests can help uncover signs of early kidney disease and monitor the condition.
Blood pressure . Your health care provider will devise a plan, which may include diet changes and medications, to keep your blood pressure as close to normal as possible. Target blood pressure is defined as less than 130/80.
Blood electrolytes. When the kidneys are not working correctly, you can develop high potassium and low calcium, phosphorus, bicarbonate, which can affect your heart’s conduction system and cause muscle aches and other complications.
Urine protein or albumin in the urine. Albumin is the main protein in the blood. When the kidneys become damaged, the holes in the filtering system of your kidneys become enlarged, allowing protein to leak into the urine. In the early stages of kidney damage, only small amounts of albumin (microalbuminuria) are found. This test is very important for people with diabetesbecause at this early stage of kidney damage, further deterioration can often be prevented by diet, exercise, and medications.
GFR (glomerular filtration rate). This is a measure of how well the kidneys are filtering blood. An estimate of your “filtering rate” is determined by a blood test called a blood creatinine test, which measures the amount of creatinine — a waste product — in your blood. This test, along with your age, body size, and gender, provides an estimate of your GFR. The GFR, or “filtering rate,” helps confirm normal or low kidney function. A score of 90 or above is normal; a score below 15 indicates kidney damage that will require dialysisor a kidney transplant. Another commonly used test to estimate GFR is a creatinine clearance. This test measures the creatinine in the blood and urine to determine kidney function.
Your health care provider may also refer you to a kidney specialist, called a nephrologist, for more specialized testing. A kidney biopsy may also be performed. During a kidney biopsy a small amount of kidney tissue is removed for microscopic exam to pinpoint the cause of kidney damage and plan treatment.
How Can I Prevent Kidney Disease?
The key to prevention or delay of severe kidney disease is early detection and aggressive intervention — while there’s still time to slow down the progression to kidney failure. Medical care with early intervention can change the course of chronic kidney disease and help prevent the need for dialysis or a kidney transplant.
Diabetes and high blood pressure account for two thirds of all cases of chronic kidney disease. By aggressively managing diabetes and high blood pressure with diet, exercise, and medications, you may be able to prevent kidney failure and help keep as much kidney function as possible.
Know Your Risks for Kidney Disease
Since diabetes and high blood pressure put you at risk of kidney disease, know where you stand with these risks. Do you have diabetes or high blood pressure? If so, are they under control?
If you can, find out if diabetes, hypertension, or kidney disease runs in your family. Certain ethnic groups, such as African-Americans, Hispanics, Pacific Islanders, and Native Americans are at higher risk of chronic kidney disease, as are senior citizens.
Get Tested Regularly
At your next checkup, and at least within the next year if you haven’t had these tests done:
Ask for a urine test to see if you have excess protein, glucose, or blood in the urine.
Ask for a blood pressure reading, to see if your blood pressure is elevated.
Ask for a fasting blood glucose test, to see if you have too much glucose (sugar) in your blood. Another blood test that can be used to determine diabetes is a hemoglobin A1C which will indicate your average blood glucose level over the past two to three months
Ask for a creatinine test. This blood test measures the amount of waste from muscle activity. When the kidneys are not working properly, the creatinine rises.
If any of these tests are abnormal, your health care provider will need to do other tests to more clearly define the problem.
Control Diabetes
If you have diabetes, work with your health care provider to keep your blood sugar levels under the best possible control. A program of diet, regular exercise, glucose monitoring, andmedicationsto control blood sugars and protect kidney function can help.
Medications for Kidney Disease
High blood pressure may be both a cause and a result of kidney disease. Your health care provider may prescribe a blood pressure drug for your kidney disease, such as an angiotensin-converting enzyme (ACE) inhibitor, such as captopril(Capoten), enalapril (Vasotec), fosinopril (Monopril), lisinopril (Prinivil, Zestril), or ramipril (Altace), or an angiotensin receptor blocker (ARB), such as azilsartan (Edarbi), eprosartan (Teveten), irbesartan (Avapro), losartan (Cozaar), olmesartan (Benicar), and valsartan (Diovan). Along with controlling blood pressure, these drugs may reduce the amount of protein in your urine, which may also help your kidneys over time.
Drugs are excreted through the kidneys, so you’ll need to consult with your health care provider before taking any medications — including over-the-counter drugs. You may be told to avoid NSAIDs, such as ibuprofen (Motrin,Advil) andnaproxen (Aleve) and COX-II inhibitors, like celecoxib(Celebrex), which are possible contributors to kidney disease. Always discuss any alternative or herbal treatments with your doctor before trying them.
Kidney Conditions
Pyelonephritis (infection of kidney pelvis): Bacteria may infect the kidney, usually causing back pain and fever. A spread of bacteria from an untreated bladder infection is the most common cause of pyelonephritis.
Glomerulonephritis: An overactive immune system may attack the kidney, causing inflammation and some damage. Blood and protein in the urine are common problems that occur with glomerulonephritis. It can also result in kidney failure.
Kidney stones (nephrolithiasis): Minerals in urine form crystals (stones), which may grow large enough to block urine flow. It’s considered one of the most painful conditions. Most kidney stones pass on their own but some are too large and need to be treated.
Nephrotic syndrome: Damage to the kidneys causes them to spill large amounts of protein into the urine. Leg swelling (edema) may be a symptom.
Polycystic kidney disease: A genetic condition resulting in large cysts in both kidneys that impair their function.
Acute renal failure (kidney failure): A sudden worsening in kidney function. Dehydration, a blockage in the urinary tract, or kidney damage can cause acute renal failure, which may be reversible.
Chronic renal failure: A permanent partial loss of kidney function. Diabetes and high blood pressure are the most common causes.
End stage renal disease (ESRD): Complete loss of kidney function, usually due to progressive chronic kidney disease. People with ESRD require regular dialysis for survival.
Papillary necrosis: Severe damage to the kidneys can cause chunks of kidney tissue to break off internally and clog the kidneys. If untreated, the resulting damage can lead to total kidney failure.
Diabetic nephropathy: High blood sugar from diabetes progressively damages the kidneys, eventually causing chronic kidney disease. Protein in the urine (nephrotic syndrome) may also result.
Hypertensive nephropathy: Kidney damage caused by high blood pressure. Chronic renal failure may eventually result.
Kidney cancer: Renal cell carcinoma is the most common cancer affecting the kidney. Smoking is the most common cause of kidney cancer.
Interstitial nephritis: Inflammation of the connective tissue inside the kidney, often causing acute renal failure. Allergic reactions and drug side effects are the usual causes.
Minimal change disease: A form of nephrotic syndrome in which kidney cells look almost normal under the microscope. The disease can cause significant leg swelling (edema). Steroids are used to treat minimal change disease.
Nephrogenic diabetes insipidus: The kidneys lose the ability to concentrate the urine, usually due to a drug reaction. Although it’s rarely dangerous, diabetes insipidus causes constant thirst and frequent urination.
Renal cyst: A benign hollowed-out space in the kidney. Isolated kidney cysts occur in many normal people and almost never impair kidney function.
Kidney Tests
Urinalysis: A routine test of the urine by a machine and often by a person looking through a microscope. Urinalysis can help detect infections, inflammation, microscopic bleeding, and kidney damage.
Kidney ultrasound: A probe placed on the skin reflects sound waves off the kidneys, creating images on a screen. Ultrasound can reveal blockages in urine flow, stones, cysts, or suspicious masses in the kidneys.
Computed tomography (CT scan): A CT scanner takes a series of X-rays and a computer creates detailed images of the kidneys.
Magnetic resonance imaging (MRI scan): A scanner uses radio waves in a magnetic field to make high-resolution images of the kidneys.
Urine and blood cultures: If an infection is suspected, cultures of the blood and urine may identify the bacteria responsible. This can help target antibiotic therapy.
Ureteroscopy: An endoscope (flexible tube with a camera on its end) is passed through the urethra into the bladder and ureters. Ureteroscopy generally cannot reach the kidneys themselves, but can help treat conditions that also affect the ureters.
Kidney biopsy: Using a needle inserted into the back, a small piece of kidney tissue is removed. Examining the kidney tissue under a microscope may help diagnose a kidney problem.