What You Should Know About the Main Side Effect of Testosterone
Testosterone replacement therapy (TRT) is one of the most effective ways to combat low testosterone levels, but it’s vital that you understand the risks associated with the treatment. As with any form of hormone replacement therapy, there are a few downsides to receiving regular injections of testosterone. But do these risks outweigh the benefits? That’s a decision you’ll have to make for yourself!
Note: Remember the purpose of TRT: to restore testosterone to NORMAL, healthy levels in the body. Ideally, testosterone levels should be normal after TRT. Even at normal levels, there is a risk of side effects.
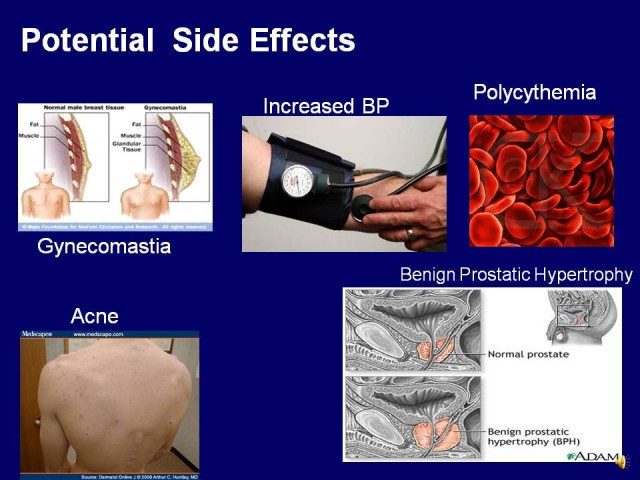
One of the primary risks of testosterone that is you need to be aware of is called polycythemia. This is a condition where your body produces too many red blood cells, also known as “high blood hematocrit levels”. Hematocrit refers to the red blood cell content in your blood. If your hematocrit levels rise, there is the fear that the blood will become too thick or viscous. This can, in turn, make it more likely that you will develop blood clots–leading to strokes, heart attacks, and other clotting events. Polycythemia is serious, potentially life-threatening if untreated.
In recent years, there has been an increased association between TRT and polycythemia. With TRT becoming a more mainstream treatment, more people are experiencing the symptoms of polycythemia, which include:
-Weakness
-Fatigue
-Headache
-Itching
-redness of the skin
-bruising
-joint pain
-dizziness
-abdominal pain
-shortness of breath
-breathing difficulty when you lie down
-numbness, tingling, or burning in the hands, feet, arms or legs
-Turning very red or “flushing” after workoutWhen polycythemia occurs, the blood becomes very thick, almost like a sludge. But instead of being able to carry MORE oxygen, the increase of red blood cells can be dangerous. The risk of clotting increases as a result of the red blood cell count increase.
Note: While there is a risk of hematocrit increase, there is no proof that TRT increases the risk of clotting events. It’s vital to be aware of the potential risk, so doctors need to be careful when prescribing TRT to men with high hematocrit levels, red blood cell disorders, and obstructive pulmonary disease. All of these things increase the risk of clotting events as a result of the hematocrit increase caused by TRT.
There are a number of factors that can increase your risk of developing this problem. According to Dr. Michael Sally, polycythemia “occurs quite frequently in people who are just on replacement testosterone.”
Age also plays a role in your polycythemia risk. Young men are far less likely to experience this problem than older men.
The mode of delivery and the dose of testosterone affect the increase in your hematocrit levels. Men who receive formulations of pharmacokinetically steady-state delivery hormones are far less likely to develop the problem than men who receive intramuscular injections of testosterone.
Topical preparations only cause the problem in up to 20% of cases. 5 to 15% of those who use testosterone patches develop polycythemia, while 10 to 20% of those using the testosterone gel develop the problem. Of course, the amount of testosterone delivered per day (50 to 100 milligrams) also affects the risk of developing polycythemia.
So what can you do about the problem? Is there any way to manage it?
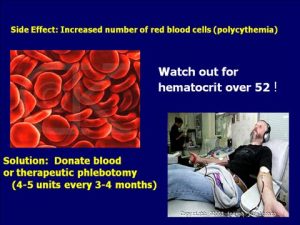
Those undergoing TRT must be aware that polycythemia is a real risk, as do their doctors. They must keep a close eye on their hemoglobin and hematocrit levels. If hematocrit rises above 52%, further examinations may be necessary.Some doctors counsel reducing or stopping the hormone treatment. However, for those who are undergoing TRT as a means of restoring healthy hormone levels, this may not be an option. Some means of managing and reducing the risk of high hematocrit levels include:
Scaling back on the amount of testosterone delivered per day or week (50mg or less)
Changing the method of administration (smaller and more frequent injections or using a gel)If these options do not work, a phlebotomy may be the answer. Removing just one pint of blood can help to lower hematocrit by as much as 3%. For those with very high hematocrit levels, the therapy may continue for weeks, gradually reducing hematocrit to safe levels over time. Some physicians even prescribe regular phlebotomies (every 8 to 12 weeks) as a means of preventing overly high hematocrit levels.
While phlebotomies are not covered by your insurance, they can be performed at any blood bank. Even if your insurance company won’t cover the cost, you can solve the problem by donating blood (provided you are free of hepatitis, HIV, and other blood-borne infections). Experts agree that donating every 2 to 3 months is safe, and it’s a good way to keep your hematocrit levels under control.
Warning: Donating more than 1 unit of blood at this frequency can lower your iron and ferritin levels. This can cause fatigue. Make sure to replace the lost iron in order to prevent anemia.
It’s recommended that you donate when you are in the 51-52% hematocrit range. However, some organizations (like the Red Cross) will reject blood with a hematocrit higher than 52%.Fun Fact: Did you know that grapefruit can help to reduce hematocrit levels? A 1988 study found that the compound naringin in grapefruits helped to reduce cell aggregation (clumps or clots), promoting the elimination of those red blood cells. The hematocrits ranged from 36.5 to 55.8% at the start and 38.8% to 49.2% at the end of the study. Those with the highest hematocrit levels noticed the greatest change as a result of the grapefruit.
More information in this link:
How to Manage Polycythemia Caused by Testosterone Replacement Therapy